Diabetes-Related Skin Conditions
Diabetes and skin health are closely tied to fluctuations in blood sugar levels. Elevated blood sugar levels can lead to dehydration, affecting the skin's ability to stay moisturized and supple. Proactive management of diabetes is crucial in mitigating the risk of skin complications.
If you or someone you know is experiencing a diabetes-related skin condition, schedule an appointment with a trusted Pinnacle Dermatology skin expert today. Our team of trusted providers is here to help you on your journey to healthy skin.
Examples of Diabetes-Related Skin Conditions





Diabetes-Related Skin Conditions Symptoms
- Acanthosis Nigricans: Dark, thick, and velvet-textured skin.
- Diabetic Blisters: On hands, toes, feet, or forearms.
- Diabetic Dermopathy: Round, brown, or purple scaly patches on shins.
- Digital Sclerosis: Thick, waxy, and tight skin on the toes, fingers, and hands.
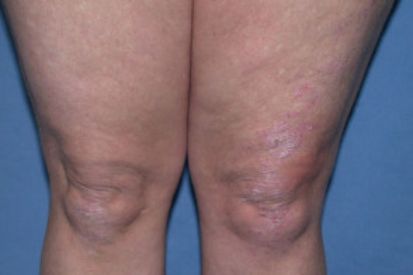
- Disseminated Granuloma Annulare: Red or reddish-brown bull’s eye rash.
- Eruptive Xanthomatosis: Red halo that itches.
- Necrobiosis Lipoidica Diabeticorum: Large, deep spots with a shiny appearance.
- Vitiligo: White patches on the skin.
Causes of Diabetes-Related Skin Conditions
- Diabetics are more susceptible to bacterial and fungal infections; allergic reactions to medications, insect bites or foods; dry itchy skin as a result of poor blood circulation; and infections from foot injuries for people with neuropathy.
- High insulin levels
- Diabetic neuropathy
- Changes in small blood vessels
- High triglycerides
- Changes in collagen and fat underneath the skin
How to Prevent Diabetes-Related Skin Conditions
Here's a list of ways to help prevent such skin complications:
- Blood Glucose Control: Maintain target blood glucose levels through regular monitoring, medication adherence, and lifestyle modifications.
- Healthy Diet: Adopt a balanced, low-sugar diet rich in fruits, vegetables, and whole grains to regulate blood sugar levels and support overall skin health.
- Regular Skin Checks: Perform regular self-examinations to detect any changes, wounds, or abnormalities early on. Promptly address any concerns with one of our dermatologists.
- Moisturize: Keep the skin moisturized to prevent dryness and cracking. Choose fragrance-free, hypoallergenic moisturizers.
- Gentle Cleansing: Use mild, fragrance-free soaps and cleansers to avoid skin irritation. Pat the skin dry after washing instead of rubbing.
- Sun Protection: Protect the skin from harmful UV rays by using sunscreen with a high SPF, wearing protective clothing, and avoiding prolonged sun exposure.
- Regular Exercise: Engage in regular physical activity, as it can help improve blood circulation and overall skin health.
- Foot Care: Inspect and care for your feet regularly, keeping them clean and dry. Wear comfortable shoes and socks to prevent friction and pressure sores.
Diabetes-Related Skin Conditions FAQs
Diabetes impacts the skin because high blood sugar levels can lead to dehydration, making the skin dry and more prone to issues. It can also affect blood flow, making it harder for the body to heal.
Maintain stable blood sugar levels, keep your skin clean and moisturized, and be attentive to any cuts or injuries. If you notice any unusual changes in your skin, consult your dermatology provider.
Diabetes can affect the body's ability to heal. Prompt care for cuts or wounds helps prevent infections, which can be more serious for individuals with diabetes.
Choose gentle, fragrance-free products and moisturizers suitable for sensitive skin. Visit our online store for high-quality medical-grade skincare. Consult with your dermatology provider for personalized recommendations.
Contact your dermatology provider promptly. Early intervention can prevent minor issues from becoming more severe. Don't hesitate to seek professional dermatological advice for any concerns about your skin.
